Cataract Surgery

Inside our eyes, we have a natural lens. The lens bends (refracts) light rays that come into the eye to help us see. The lens should be clear.
Cataracts are the major cause of vision loss in the United States. Symptoms can include blurry, hazy vision that worsens over time as well as sensitivity to glare.
Research has shown that treatment in the form of specific lifestyle, diet and supplement choices can support overall lens health.
Download Outpatient Post Op Instructions
A cataract appears as an opaque spot on the lens of the eye that obstructs vision. It may seem as though you are looking through a hazy cloud.
The density of the cataract typically increases over time so the effect on your vision will vary depending on the cataract density and the location of the cataract on the lens.
Many people first experience a general blurriness of vision requiring more light to read by, and/or more difficulty reading street signs. Depth perception can often be affected resulting in an added risk of falling for seniors.
Cataract Surgery in Houston, TX
Here are some vision changes you may notice if you have a cataract:
- Having blurry vision.
- Seeing double (when you see two images instead of one).
- Being extra sensitive to light.
- Having trouble seeing well at night, or needing more light when you read.
- Seeing bright colors as faded or yellow instead.
Aging is the most common cause. This is due to normal eye changes that happen starting around age 40.
That is when normal proteins in the lens start to break down. This is what causes the lens to get cloudy. People over age 60 usually start to have some clouding of their lenses. However, vision problems may not happen until years later.
Other reasons you may get cataracts include:
- Having parents, brothers, sisters, or other family members who have cataracts.
- Having certain medical problems, such as diabetes.
- Having had an eye injury, eye surgery, or radiation treatments on your upper body.
- Having spent a lot of time in the sun, especially without sunglasses that protect your eyes from damaging ultraviolet (UV) rays.
- Using certain medications such as corticosteroids, which may cause early formation of cataracts.
Most age-related cataracts develop gradually. Other cataracts can develop more quickly, such as those in younger people or those in people with diabetes. Doctors cannot predict how quickly a person’s cataract will develop.
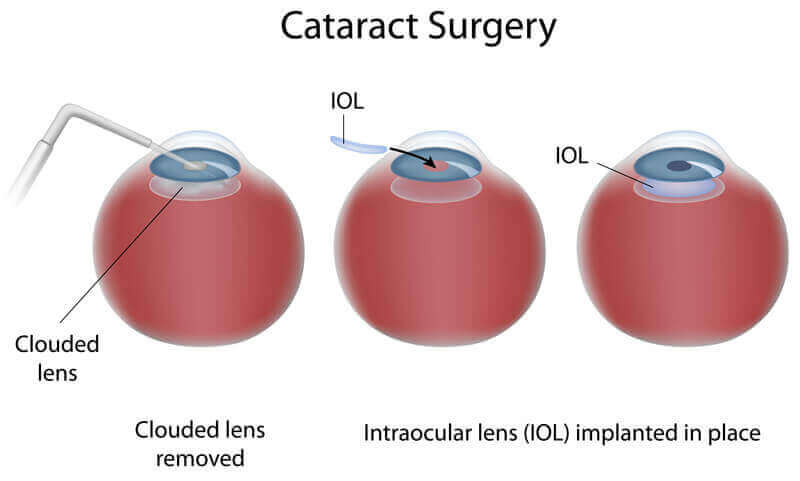
Cataract surgery is an operation to remove your eye’s lens when it is cloudy.
The purpose of your lens is to bend (refract) light rays that come into the eye to help you see. Your own lens should be clear, but with a cataract it is cloudy. Having a cataract can be like looking through a foggy or dusty car windshield. Things may look blurry, hazy or less colorful.
The only way to remove a cataract is with surgery. Dr Hung Le will recommend removing a cataract when it keeps you from doing things you want or need to do.
During cataract surgery, your cloudy natural lens is removed and replaced with a clear artificial lens. That lens is called an intraocular lens (IOL). Your ophthalmologist will talk with you about IOLs and how they work.
Before surgery:
Your surgeon will measure your eye to determine the proper focusing power for your IOL. Also, you will be asked about any medicines you take. You might be asked not to take some of these medicines before surgery.
You may be prescribed eye drop medicines to start before surgery. These medicines help prevent infection and reduce swelling during and after surgery.
The day of surgery:
Your ophthalmologist may ask you not to eat any solid food at least 8 hours before your surgery.
Cataract removal surgery may be done in an outpatient surgery center or in a hospital. Here is what will happen:
- You may be prescribed eye drop medicines to start before surgery. These medicines help prevent infection and reduce swelling during and after surgery.
- Your eye will be numbed with eye drops or with an injection around the eye. You may also be given a medicine to help you relax.
- You will be awake during surgery. You may see light and movement during the procedure, but you will not see what the doctor is doing to your eye.
- Dr. Le looks through a special microscope. She creates tiny incisions (cuts, created by laser or a blade) near the edge of your cornea. The surgeon uses these incisions to reach the lens in your eye. Using very small instruments, he or she will break up the lens with the cataract and remove it. Then she puts your new lens into place.
- Usually. Dr Le will not need to stitch the incisions closed. These “self sealing” incisions eventually will close by themselves over time. A shield will be placed over your eye to protect it while you heal from surgery.
- You will rest in a recovery area for about 15–30 minutes. Then you will be ready to go home.
Days or weeks after surgery:
- You will have to use eye drops after surgery. Be sure to follow your doctor’s directions for using these drops.
- Avoid getting soap or water directly in the eye.
- Do not rub or press on your eye. Your ophthalmologist may ask you to wear eyeglasses or a shield to protect your eye.
- You will need to wear a protective eye shield when you sleep.
- Dr. Hung Le will talk with you about how active you can be soon after surgery. He will tell you when you can safely exercise, drive or do other activities again.
Like any surgery, cataract surgery carries risks of problems or complications. Here are some of those risks:
- Eye infection.
- Bleeding in the eye.
- Ongoing swelling of the front of the eye or inside of the eye.
- Swelling of the retina (the nerve layer at the back of your eye).
- Detached retina (when the retina lifts up from the back of the eye).
- Damage to other parts of your eye.
- Pain that does not get better with over-the-counter medicine.
- Vision loss.
- The IOL implant may become dislocated, moving out of position.
Cataract surgery will not restore vision lost from other eye conditions such as macular degeneration, glaucoma, or diabetic retinopathy.
Dr Hung Le will talk with you about the risks and benefits of cataract surgery.
Posterior Capsular Opacification
Your vision could become cloudy or blurry weeks, months or years after cataract surgery. This is not unusual.
Your doctor might call this a “posterior capsular opacification (or PCO).” It’s also called “secondary cataract” or “scar tissue.” It’s not like a scar you get on your skin. But because it happens after the eye has healed from cataract surgery, some people think of it as a scar. It happens when a membrane called the posterior capsule becomes cloudy.
It might help to think of the posterior capsule as a transparent pocket. It holds your IOL in place. It also once held your eye’s natural lens (what became the cataract) in place. If you notice cloudy vision again, you might need to have a laser procedure.
The laser creates an opening in the cloudy capsule and is called a posterior capsulotomy (or a YAG laser capsulotomy). This procedure helps restore clear vision.
Cataract surgery costs are generally covered by Medicare if you are Medicare eligible. Private insurance usually covers cataract surgery as well.
Medicare will cover your costs if your vision tests at a certain level of acuity or clarity. Private insurance plans may have similar vision requirements. If your surgery is covered you may still have some costs. Special types of IOLs will cost more. Choosing to have cataract surgery before your vision has deteriorated enough will cost more.
In certain cases, it might be possible to get coverage before you meet the age or vision requirements. Talk with your ophthalmologist if you are considering having early cataract surgery.
What do you do if you don’t have Medicare or private insurance coverage? You may still be able to reduce and manage the cost of cataract surgery.
Ask about payment plans through your doctor’s office. See if your employer offers flexible spending accounts that can help. Your ophthalmologist can help you learn more about costs of cataract surgery. Discuss your options for affording the procedure.
Yes, however, extra attention needs to be paid towards monitoring the intraocular eye pressure (IOP). The IOP can rise following cataract surgery for any patient, even those without glaucoma. Anyone who undergoes cataract surgery with glaucoma should carefully follow the instructions their cataract surgeon provides to them. Taking your glaucoma medication before and after cataract surgery, as well as attending all scheduled post-operative visits, is crucial.
In many cases, yes! Cataract surgery removes the eye’s natural lens and replaces it with an artificial one called an intraocular lens or IOL. Depending on which one you pick, you could significantly improve your vision. Some IOLs specifically aim to improve nearsightedness, farsightedness, and astigmatism. Schedule an appointment to learn more about what IOL might be right for you!













